Does Health Insurance Cover Covid Rapid Test
Waiver of cost share is effective from Feb. Those self-funded employer plans do not have to conform to any.

Antigen And Molecular Tests Types Of Covid 19 Tests
Its 219 for same-day results or 299 for results in one hour.

Does health insurance cover covid rapid test. The cost of a COVID-19 test should be fully covered by health insurance and a person doesnt have to have symptoms or exposure to someone. Members to contact WPA for prior approval. Not all tests are covered by insurance but since the passage of the Families First Coronavirus Response Act in March many people should have coverage for coronavirus testing.
If your insurance does not cover the test the cost is 135. DM Covid-19 Test conducts curbside tests at their Columbia office. Covers a test to see if you have coronavirus officially called coronavirus disease 2019 or COVID-19.
These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan. Rapid point of care antigen tests where results are available within a few minutes Home test kits when ordered by a licensed healthcare provider. Tests must be provided or ordered by a healthcare provider licensed or authorized to provide or order COVID-19 tests.
Your costs in Original Medicare You pay nothing for this test when you get it from a laboratory pharmacy doctor or hospital and when Medicare covers this test in your local area. Members Aetna is here to keep you informed during the coronavirus COVID-19 pandemic. For example tests conducted for return to work purposes or travel are generally not covered.
LabCorp will mail your specimen kit to you. Home testing for Covid-19 for members cost 99 20 telephone consultation fee results in 5-7 days. Some that charge travelers for rapid and PCR tests and some that offer complimentary screenings for travelers.
Collect your own specimen by following the detailed instructions. 2 Rapid-result tests can be pricey costing up to 250 and often arent covered by health insurance. Based on information gathered from the five largest health insurance companies in the United States there is no limit on how many free COVID-19 tests an insured member can receive.
Many airports are now offering test sites. If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. Like the coronavirus vaccine testing for COVID-19 is free to anyone in the United States including people without health insurance.
17 2021 for in-network and out-of-network tests. NHS approved Covid-19 antibody tests where a medical professional recommends it is clinically necessary are also covered. Will be covered by Cigna cost share waived.
When are COVID-19 tests not. Most health insurance plans do not cover COVID-19 tests for reasons other than diagnosis or treatment by a health care professional. 4 2020 through the national public health emergency period currently scheduled to end Oct.
Complete an online screening. Waiver of cost share is subject to state regulations. State variations and regulations may apply.
Federal law requires insurers to fully cover coronavirus tests ordered by health care providers meaning the doctor cannot apply a deductible or co-payment to the service. HealthPartners covers 100 of the cost for all testing that meets the above guidelines which most testing does. Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a.
Youll need a negative COVID-19 viral test to re-enter the United States as well. This includes PCR testing which takes a sample of the mucus from a persons nose or throat as well as saliva testing which takes the sample from a persons saliva to determine if a person has an active infection of the SARS-CoV-2 virus the virus that causes COVID-19. Commonly known as COVID-19 PCR test or simply PCR the State Health Plan covers this test at no member cost when prescribed by a healthcare provider for individuals who are symptomatic and for those who have been exposed to COVID-19 and are concerned about infection for the purpose of identifying and treating the disease.
UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing. Coronavirus COVID-19 Health Insurance FAQs. And over at Allianz Global Assistance which offers COVID-19 insurance and assistance for clients who test positive for COVID-19 while travelling a COVID-19 test will only be.
Employer sponsored self-funded health plan are regulated by the US Department of Labor under ERISA. Blue Shield and Blue Shield Promise cover these diagnostic tests. Provide your Cigna insurance information.
UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment. The Connecticut Department of Insurance regulates fully insured health insurance plans issued in the State of Connecticut only. Government pre-paid for COVID-19 vaccines and required COVID-19 vaccines be made available at no out-of-pocket costs regardless of whether the vaccine.
Federal law requires all private insurance plans to cover the entire cost associated with approved COVID-19 testing so long as the test is deemed medically appropriate. Whether you conduct your COVID-19 test at home or at a clinic if its ordered by a licensed health care professional who believes its medically appropriate then federal legislation requires your private health plan to cover the cost said Sabrina Corlette a research professor who studies health insurance policy at the Center on Health Insurance Reforms at Georgetown University. Visit our FAQ page for answers to the most frequently asked questions regarding COVID-19 testing and treatment and to get the latest information.
Standard PCR tests sent to a lab. Tufts Medical Center conducts tests in Boston with results in 48-72 hours.

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff

Rapid Covid 19 Testing Vitalcare Primary And Family Care

Rapid Covid Tests What You Should Know About Accuracy
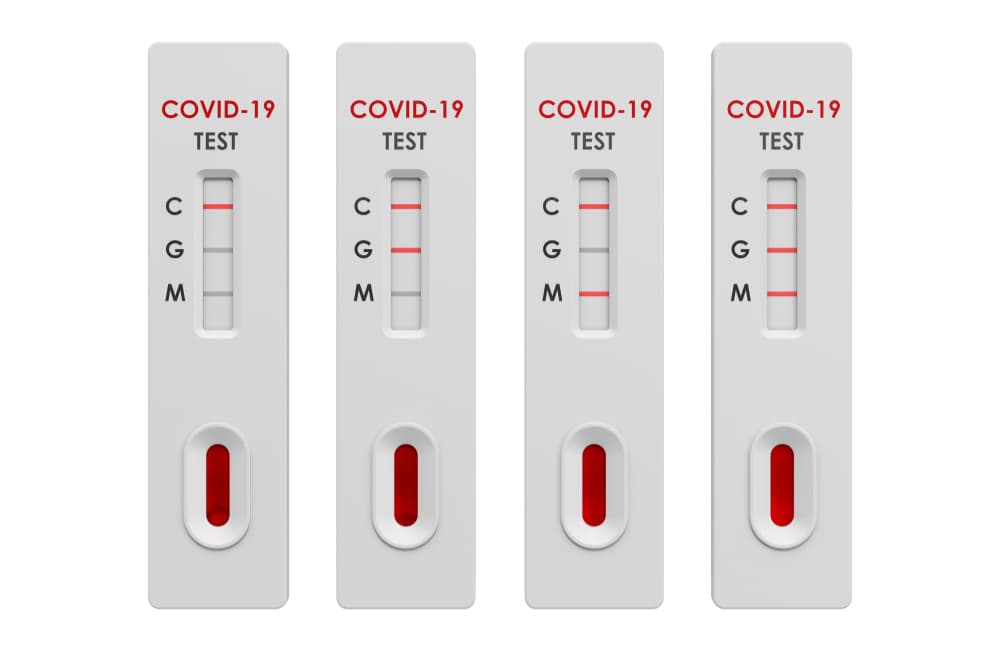
Sars Cov 2 Covid 19 Diagnosis By Igg Igm Rapid Test Clinisciences

Moh Antigen Rapid Test Art Self Test

Rapid Covid 19 Testing Urgent Care Omaha Bellevue Ne Clinics
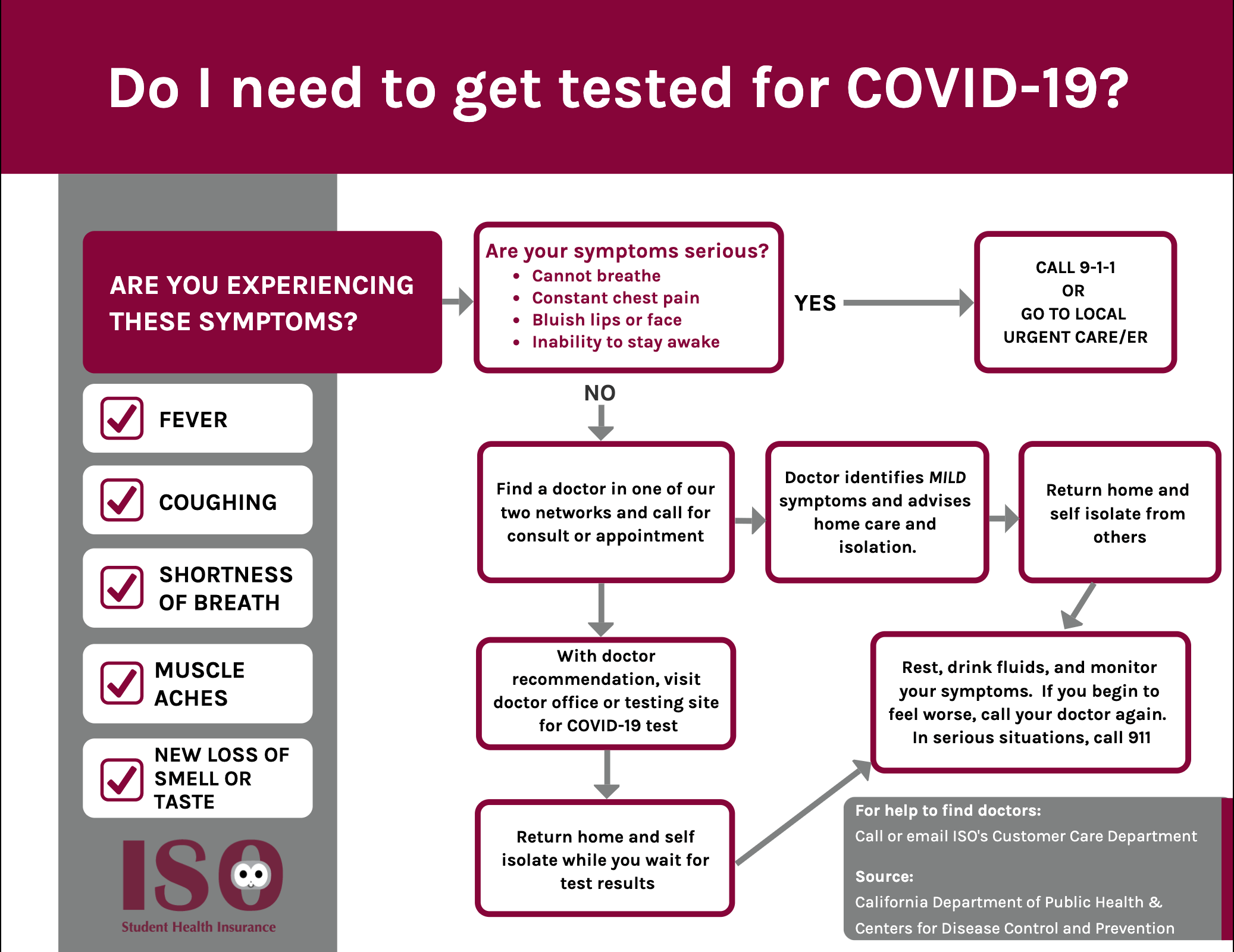
Iso International Student Insurance

Sars Cov 2 Covid 19 Diagnosis By Igg Igm Rapid Test Clinisciences

Home Tests Could Help In The Fight Against The Coronavirus So Where Are They The Washington Post

Antigen And Molecular Tests Types Of Covid 19 Tests
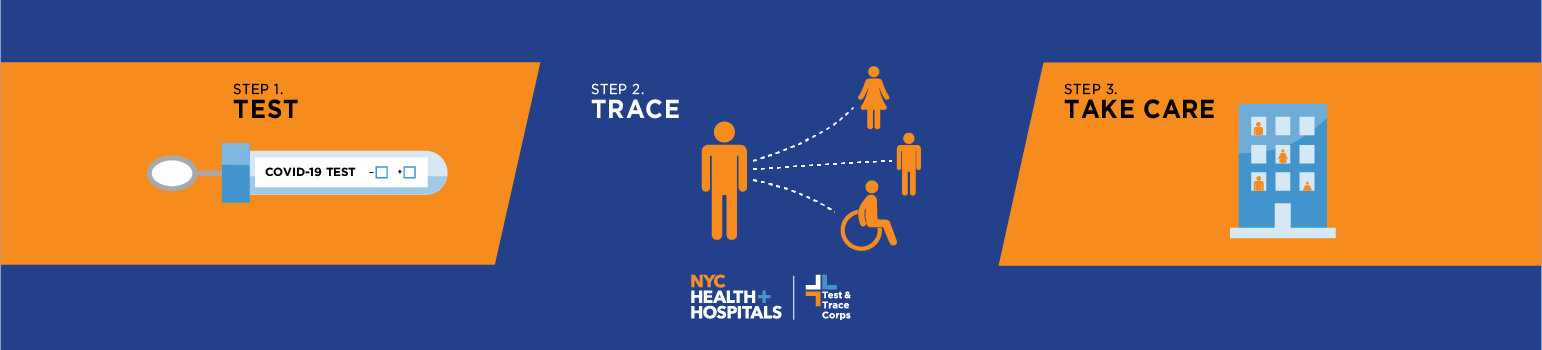
Test Trace Corps Testing Nyc Health Hospitals

Test Yourself For Covid 19 With Our Rapid Antigen Self Test Youtube

Mass Testing For Covid 19 January Update On Lateral Flow Tests Post
Klm Faq Travelling By Aircraft In The Time Of Coronavirus Klm
.png)
Insurance And Takaful Industry Covid 19 Testing Fund For Medical Insurance Policyholders

Testing For Covid 19 Faqs Blue Shield Of Ca
Antigen Testing For Covid 19 Is Now Available In South Africa Discovery

How Americans Can Get A Covid Test In Mexico The Washington Post


Posting Komentar untuk "Does Health Insurance Cover Covid Rapid Test"