Does My Insurance Cover Covid Testing Cigna
So if you cant find your insurance on our list give your local CityMD a call and well provide coverage answers fast. Cigna is waiving out-of-pocket costs for COVID-19 visits with in-network providers whether at a providers office urgent care center emergency room or via virtual care through the Public Health Emergency PHE period currently scheduled to end on October 18 2021.
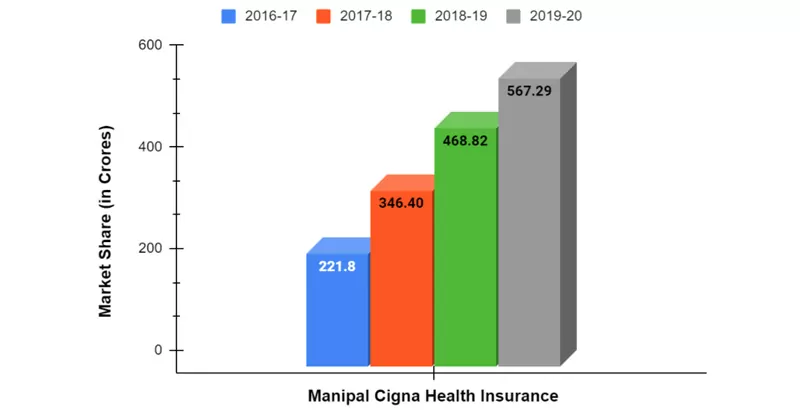
Manipal Cigna Health Insurance Plans Reviews And Premium Calculator
Does Cigna Cover Covid testing at urgent care.
Does my insurance cover covid testing cigna. Complete an online screening. FOX31 was told thats to cover. Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles.
Insurers must cover the cost of the diagnostic testing even if the person just wants for example to be sure that they dont have COVID before visiting friends or family members insurers are not required to cover the cost of widespread COVID testing. CI customers will have access to coronavirus COVID-19 testing as prescribed. State variations and regulations may apply.
Per guidance from the Centers for Medicare Medicaid Services CMS the Department of Labor and the Department of the Treasury all Commercial Medicaid and Medicare plans must cover COVID-19 serological antibody testing with no cost-sharing. Many insurers youve seen in the news like Blue Cross Blue Shield Aetna and Cigna have announced that if you or someone in your. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021.
If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. Per usual policy Cigna does not require three days of inpatient care prior to transfer to an. You may also have to fill out a screening form.
CMS has clarified that insurers cannot limit this coverage only to people who are symptomatic or who have a history of exposure to someone diagnosed with COVID-19. We do not cover the cost of antibody testing. Anthem does not specify a limit on the number of COVID-19 tests it will cover.
Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a. The company will reimburse health care providers at Cignas in-network rates or Medicare rates as applicable. You will need an appointment for most of these sites.
All comprehensive health insurance companies must cover 100 of coronavirus testing and treatment according to the Federal stimulus package known as the Coronavirus. In COVID-19 admissions Cigna will allow direct emergent or urgent transfers from an acute inpatient facility to a second acute inpatient facility. A person with no insurance wouldve been charged 85.
Provide your Cigna insurance information. COVID-19 testing at temporary or pop-up testing sites is covered by Blue Shield and Blue Shield Promise without out-of-pocket costs. Self-initiated at-home specimen collection kits that are FDA-approved such as the Pixel by LabCorp testing kit will be covered by Cigna cost share waived.
For further details on testing and our policy please refer to Will you pay for the cost of COVID 19 testing below. BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. Yes most likely you can still get health insurance if you have been diagnosed with COVID-19 but the insurance company might exclude Coronavirus from your coverage.
Then COVID drive-up charges insurance companies 30 for what the bills calls an OBGYN Fee. You will be responsible for any testing costs related to non-diagnostic COVID-19 tests and the cost of the visit associated with the test will be covered according to your plans normal cost-share. Cigna covers out-of-pocket expenses for a covered COVID-19 diagnostic visit and testing with no customer cost share through the Public Health Emergency PHE period currently scheduled to end on October 18 2021.
If you are worried that you may have been exposed to COVID-19 please contact us. This is because insurance companies will consider COVID-19 as a pre-existing condition. The CARES Act also requires insurers to cover the testing without any prior authorization requirements or imposing cost-sharing on patients.
Since the legislation was passed on March 18 2020 all forms of public and private insurance are required to cover the costs of COVID-19 testing using tests approved by. The treatments that Cigna will cover for COVID-19 are those covered under Medicare or other applicable state regulations. While we take most Commercial Managed Medicaid Medicare Advantage and exchange plans understanding your exact coverage can be confusing.
We only cover the cost of PCR testing when requested by a medical professional. Oscar does not cover COVID-19 antibody tests if they are administered outside of these settings because they are not used to diagnose COVID-19 or determine a course of treatment. We are now taking Fidelis and MetroPlus in New York.

Manipal Cigna Health Insurance Plans Reviews And Premium Calculator

Cigna Requires Employees Returning To Office To Be Fully Vaccinated Reuters
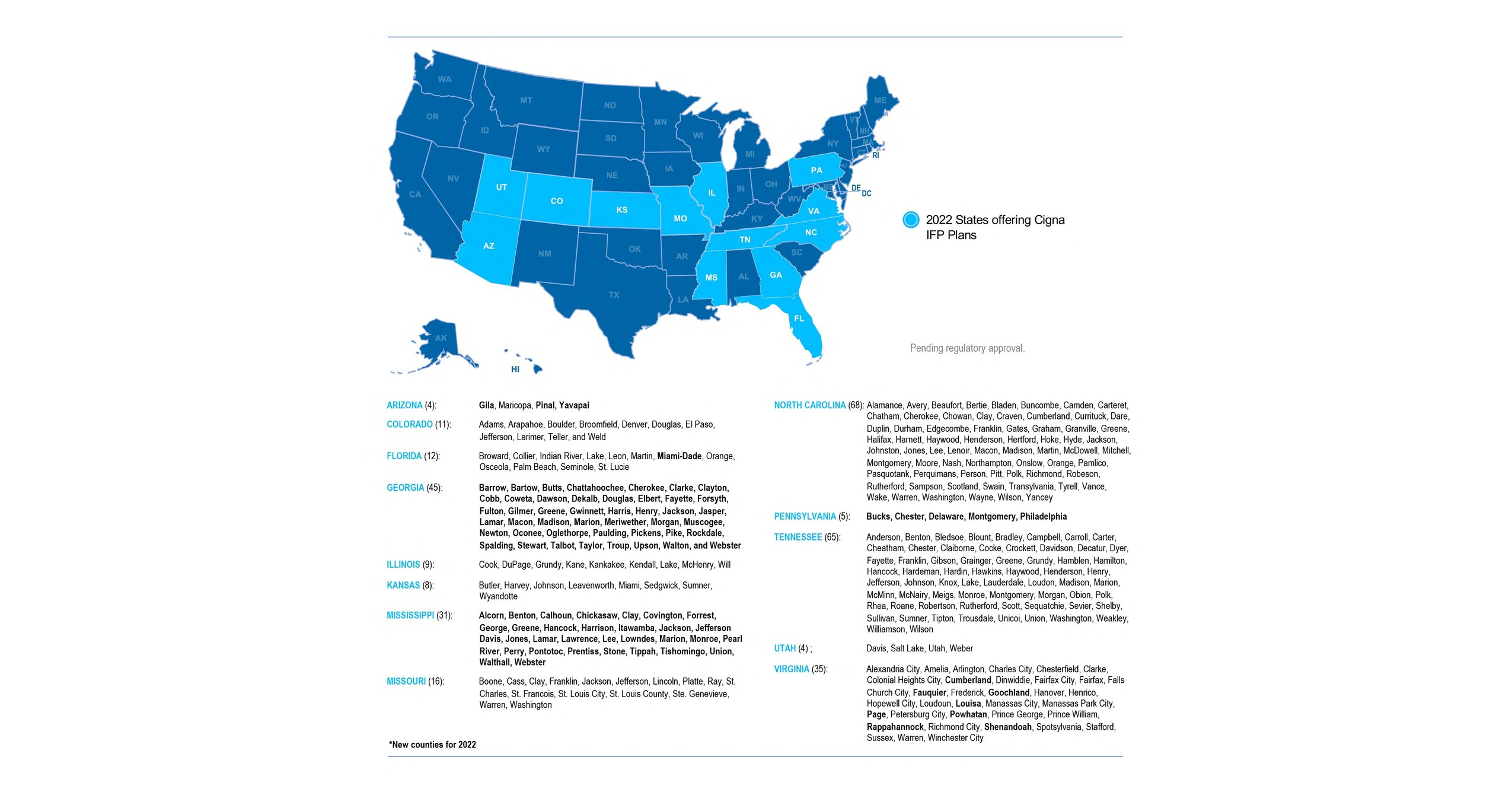
Cigna Expands Enhances Aca Marketplace Plans To Increase Access To Quality Care In More Communities
Find A Doctor In The Cigna Network Healthpartners

Cigna Protects Its Workforce By Requiring Covid 19 Vaccinations Or Testing For Employees Entering U S Worksites
/cdn.vox-cdn.com/uploads/chorus_image/image/69734462/CareCube_Park_Slope.0.jpg)
Surprise Covid Test Bills Prompt Complaint To Ny Attorney General The City

Guidelines For Working During Covid 19 Cigna

Cigna And Humana Waive Coronavirus Treatment Costs

What To Know About Coronavirus Your Insurance Utah Insurance Department

Ways To Avoid High Costs Of Rapid Covid 19 Tests Video Wsmv Com

Cigna Humana Waive Patient Out Of Pocket Costs For All Coronavirus Treatment

Most People Won T Have To Pay For Covid 19 Testing Coronavirus
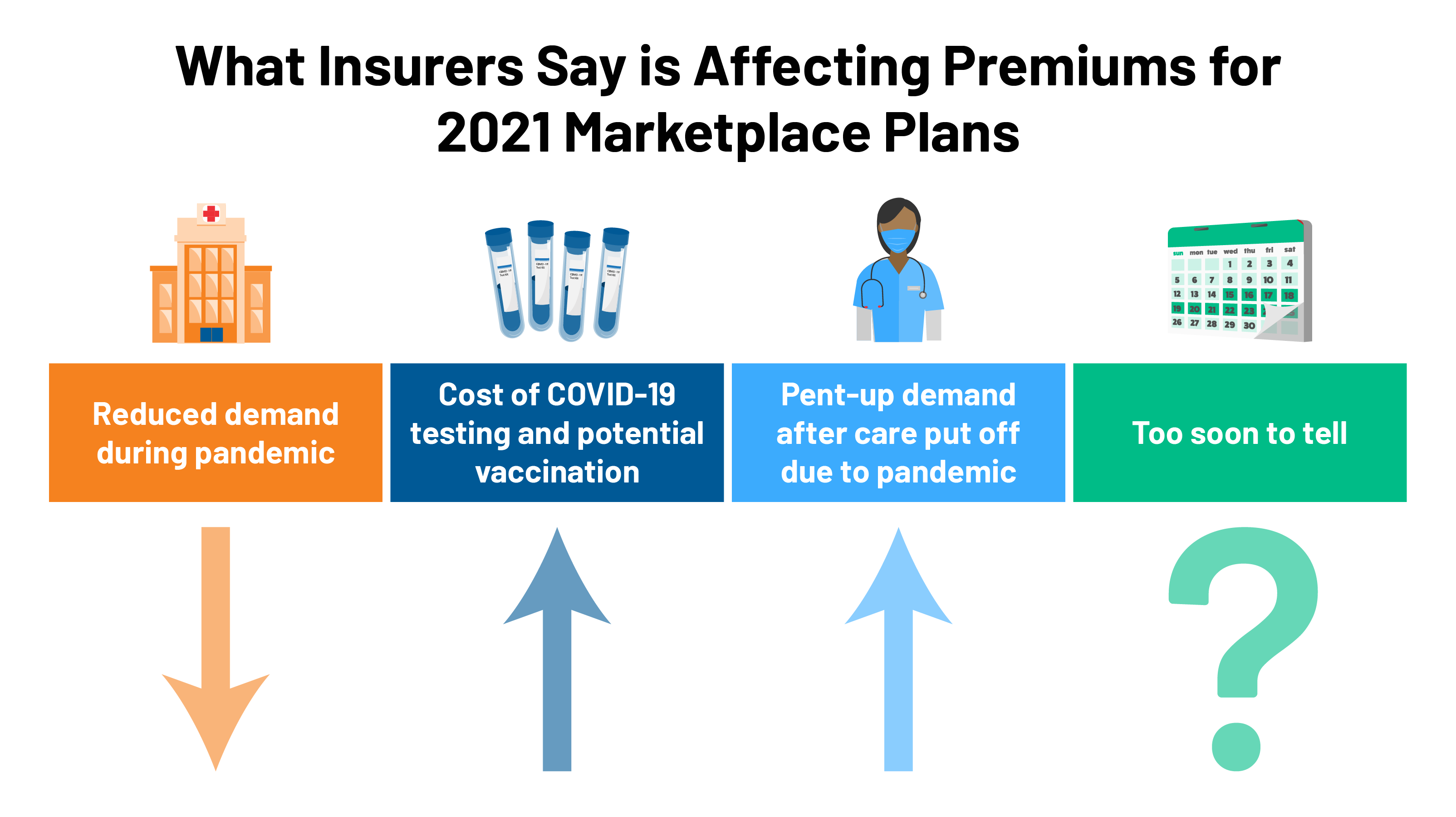
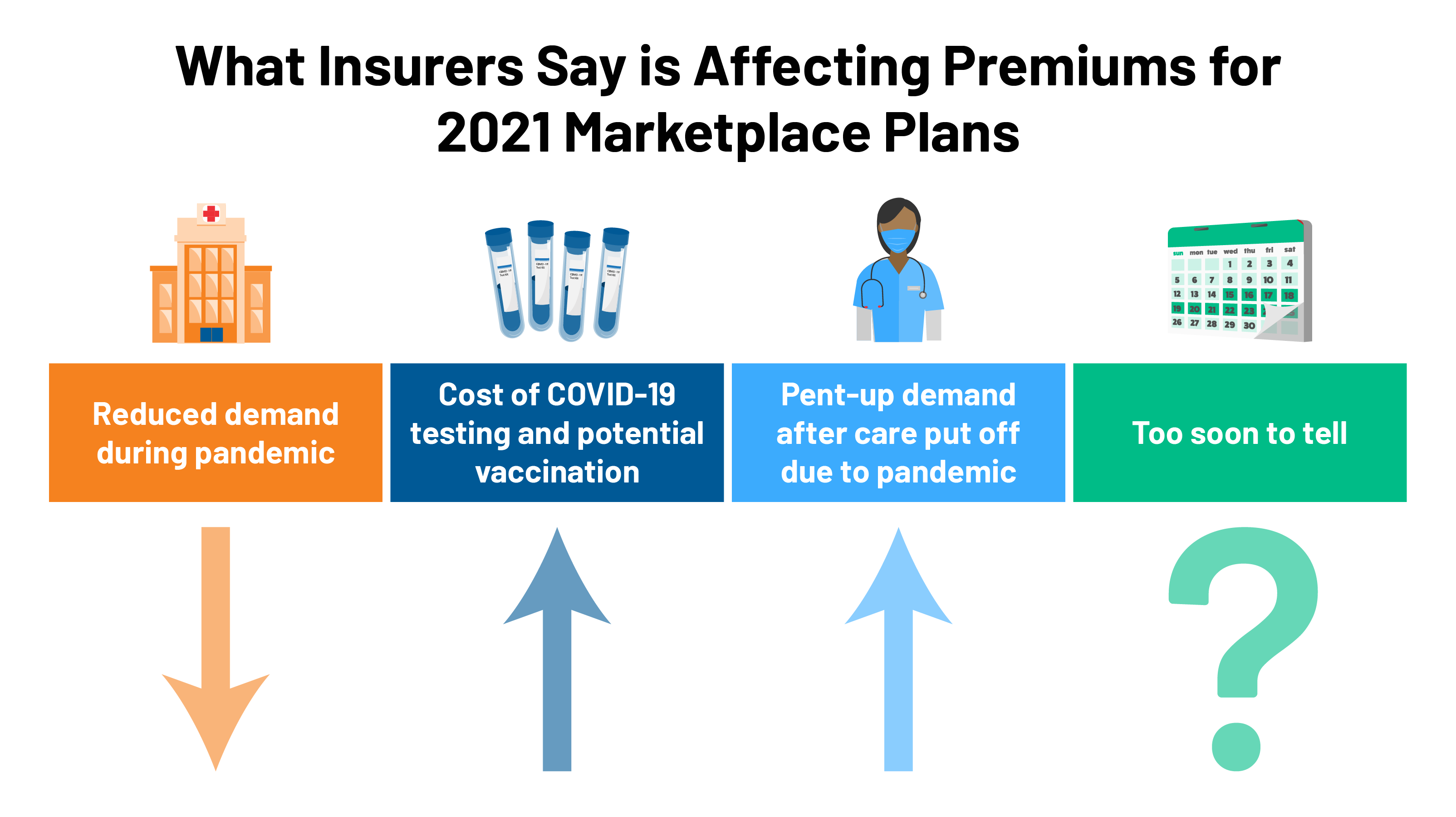
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff

Pcr Test In Puerto Vallarta Available In Three Locations Hospital Cmq

Dental Benefits Employees Cone Health
Posting Komentar untuk "Does My Insurance Cover Covid Testing Cigna"