Insurance Coverage For Proton Therapy
Similar to Part A you will be required to pay up to your annual deductible and you may also be responsible for a copayment which is a set cost for visiting a certain provider or attending a specific appointment. Insurance Coverage for Adjuvant Proton Therapy in the Definitive Treatment of Breast Cancer.
AFTER A SUCCESSFUL APPEAL If a patient receives an approval for their treatment after an appeal make sure that the costs are covered at the rate described in their plan.

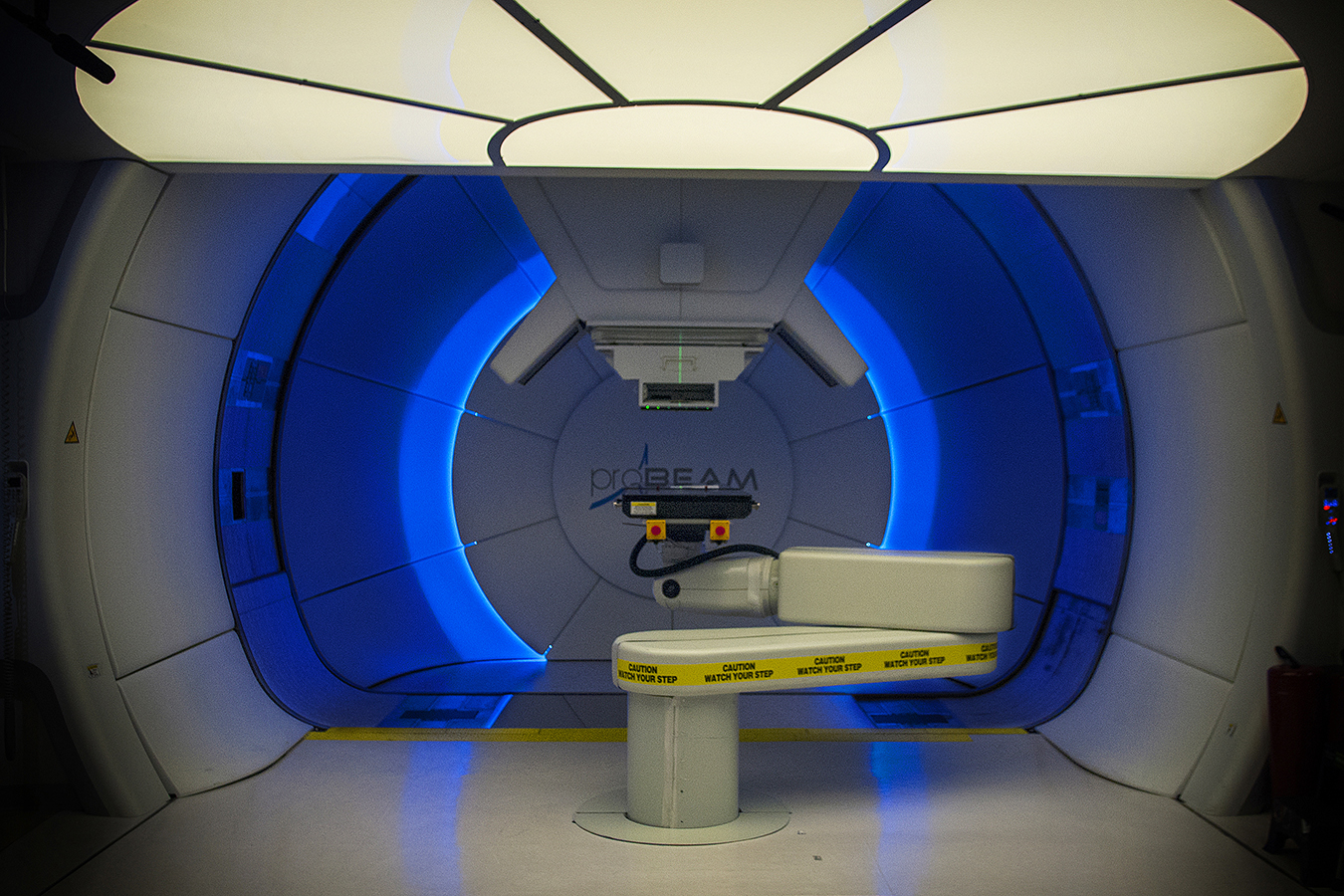
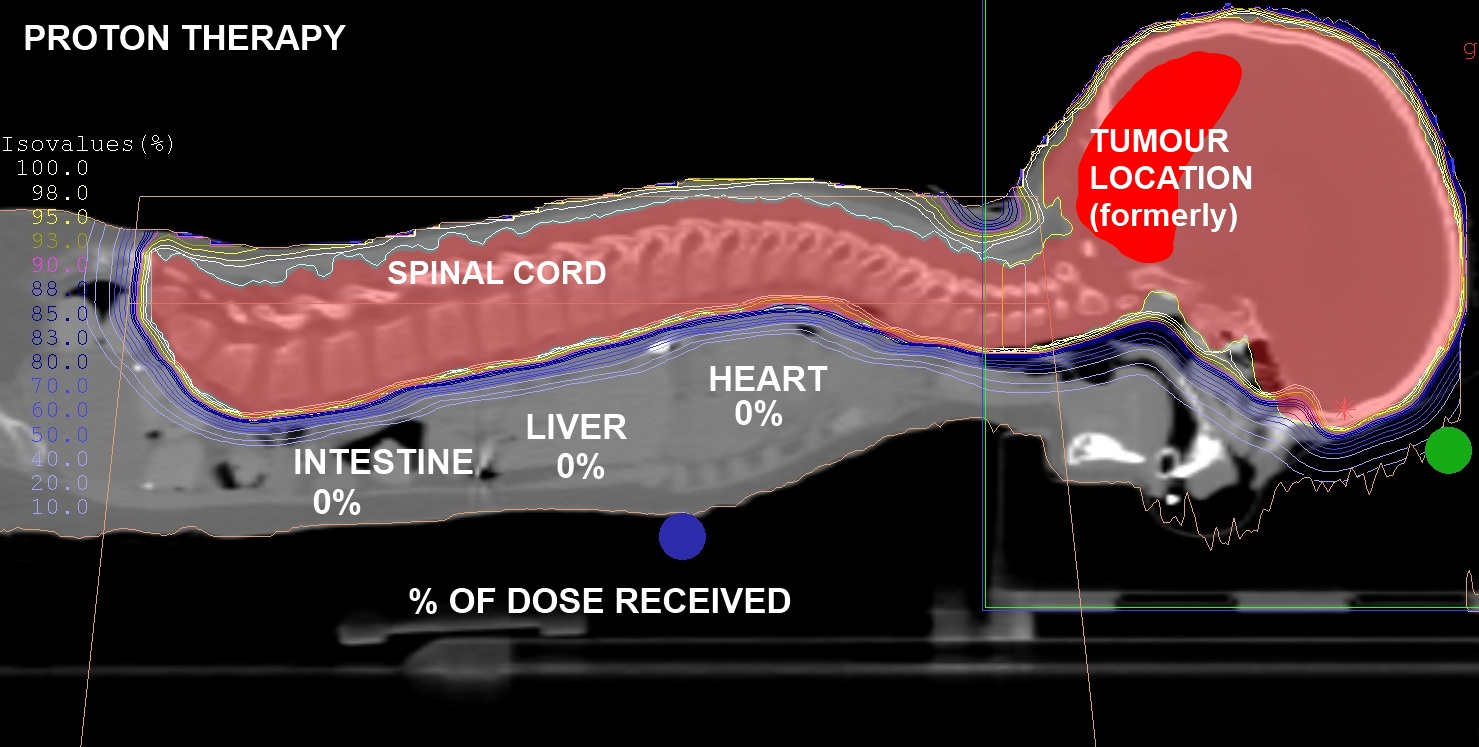
Insurance coverage for proton therapy. Expanding Insurance Coverage for Proton Therapy 1. Proton beam radiation therapy PBRT is intended to deliver higher more targeted radiation with less damage to collateral healthy tissue than external beam radiation therapy EBRT using photons x -rays when used to treat solid tumors. Blue Cross Blue Shield of Massachusetts now covers proton therapy for patients who have specific cancers and are enrolled in prospective clinical studies including prostate and left-sided breast cancers owing to the proximity of the heart which might facilitate timely completion of these studies.
That proton therapy is investigational even though it has been in use for more than 50 years and has been used in well over 100 000 patients worldwide. Private insurance companies generally cover proton therapy on a case-by-case basis depending on the type of tumor being treated previous treatments medical history and other factors. Others including UnitedHealthcare cover the therapy for additional conditions including skull.
At ProCure we are in-network with many insurance providers including Medicare Medicaid Aetna. The cost of proton therapy varies based on your condition medical history number of treatments insurance coverage type of benefit plan and other factors. Proton Therapy was approved by the FDA in 1988 and most cancer diagnoses have been covered by Medicare since 1997.
Some insurers such as Cigna cover proton therapy only for cancer of the eye. These findings epitomize the catch-22 affecting all proton therapy providers. If the insurer claims that proton is experimental and using that as the denial reason it is the easiest denial to appeal Note.
Of bad-faith insurance in its denial of coverage for proton beam radiation therapy. In this context we examined insurance coverage decisions at our facility from 2010 to 2015. Some insurance companies that did not cover proton therapy occasionally approved and paid for treatment with PT.
If your insurance carrier does pay for proton therapy patients often incur little or no net out-of-pocket expenses after deductibles and annual maximum payments are met. Unfortunately insurance companies sometimes prevent cancer patients from receiving the medical attention they need by denying coverage for proton therapy. Proton beam therapy PBT holds promise for pediatric patients but level 1 evidence is not available.
Proton beam therapy is covered by Medicare and many private insurance companies. While proton beam cancer therapy treatment is covered by Medicare private insurance coverage varies. The Broken State of Patient Access to Proton Therapy May 25 2018.
Authors Anand Shah 1 Kelsey I Ricci 2 Jason A Efstathiou 3 Affiliations 1 Department of. There are various reasons insurance companies will deny coverage for proton therapy including claiming it is experimental or not medically necessary for your particular cancer diagnosis. Major insurance companies deny coverage because of the lack of level 1 evidence for proton therapy22 31 yet the very trials needed to generate such data cannot accrue because of lack of coverage32 33 The National Institutes of Health and National Cancer Institute attempted to address this issue by.
Some companies do not reimburse for the service or only cover treatment for certain diagnoses. In other words the proton beam facilities seek to treat more common cancers. As of this print date Medicare covers proton therapy for prostate cancer at 80 percent of the usual and prevailing fee and Medicare never covers anything experimental.
Coverage is determined on a case by case basis depending on your diagnosis medical history and other factors. A class action lawsuit filed in October 2020 by a Florida man accuses Aetna Life Insurance Co. With or without coverage a lengthy process of medical review and decision appeal might ensue before a final decision was made to approve or not approve treatment with PT.
Lin Liao Shaaban et al. If proton therapy is being conducted in an outpatient facility Medicare Part B may help cover the costs. Learn how New York Proton Center is taking all.
If you are currently discussing these decisions your doctor may recommend proton therapy as part of your treatment. Lawler M Banks I Law K et. PBT was initially denied for 11 of pediatric cases.
Comparative toxicities and costs of preoperative chemoradiotherapy of IMRT and proton beam. Proton therapy may still provide the life-saving treatment you need. Nevertheless proton therapy tends to be more expensive than traditional radiation and is still not covered by many insurance companies.
Proton therapy is typically covered by Medicare and many commercial insurance providers. Despite the legislative eff orts to ensure a minimum standard for insurance coverage of patients in clinical trials how private payers address these obligations diff ers between states. Still some companies may be ignoring this information and even go so far as to disregard letters from patients doctors regarding the efficacy and necessity of the treatment.
Proton therapy is even covered under Medicare as a safe and effective treatment for prostate cancer. To determine factors that influence insurance approval for breast cancer patients for whom adjuvant proton therapy PT is recommended. In addition to Medicare private insurance companies such as Blue Cross Aetna United Healthcare and Cigna offer coverage for these cancersbut some of them are relatively rare.
United Healthcare Sued Over Proton Therapy Denials. Insurance coverage for proton therapy Lancet Oncol. Epub 2016 Apr 27.
Some insurers including Cigna Independence Blue Cross and Blue Cross Blue Shield of Florida cover proton therapy for selected cancers being studied sometimes with study participation.

Fukushima Radiation Causing U S Insurance Companies To Exclude All Coverage For Radiation Claims Radiation Exposure Acute Radiation Syndrome Radiation
Why Proton Therapy Proton Therapy Partners

Proton Beam Therapy Latest Technology In Cancer Care Onco Com

Laptop Battery Booster Intel Haswell Chip Is Business Traveler S Dream Intel Innovation Technology Technology

Pin On Johns Journey To A Cure For Prostate Cancer Proton Therapy
Boom In Proton Therapy Is A Bust For Some Blame A Shortage Of Patients California Healthline

Proton Beam Therapy Program Overview Mayo Clinic Protons Therapy Mayo Clinic

What To Do When Your Health Insurance Won T Pay The Bills Health Insurance Best Health Insurance Cheap Health Insurance

Cost Insurance Coverage Of Proton Therapy For Cancer California Protons

Proton Beam Therapy Program Frequently Asked Questions Mayo Clinic
Why Proton Therapy Proton Therapy Partners

The Insurance Approval Process For Proton Radiation Therapy A Significant Barrier To Patient Care International Journal Of Radiation Oncology Biology Physics

Amid Questions About Cost And Access Proton Therapy Set For Big Moment Of Change

The Global Radiotherapy Devices Market Is Expected To Exceed More Than Us 7 5 Billion By 2022 And Wil Radiation Therapy Medical Oncology Concussions Treatment
Proton Therapy Now Covered By Most Health Insurance Companies In Czech Republic Imaging Technology News

Gamma Knife Radiosurgery Is A Surgical Technique In Which A Single Dose Of Radiation Is Used To Cancer Radiation Therapy Medical Conditions Radiation Treatment

Judge Rips Insurance Company For Immoral Barbaric Cancer Denials Cnn


Posting Komentar untuk "Insurance Coverage For Proton Therapy"