Does Va Insurance Cover Covid Testing
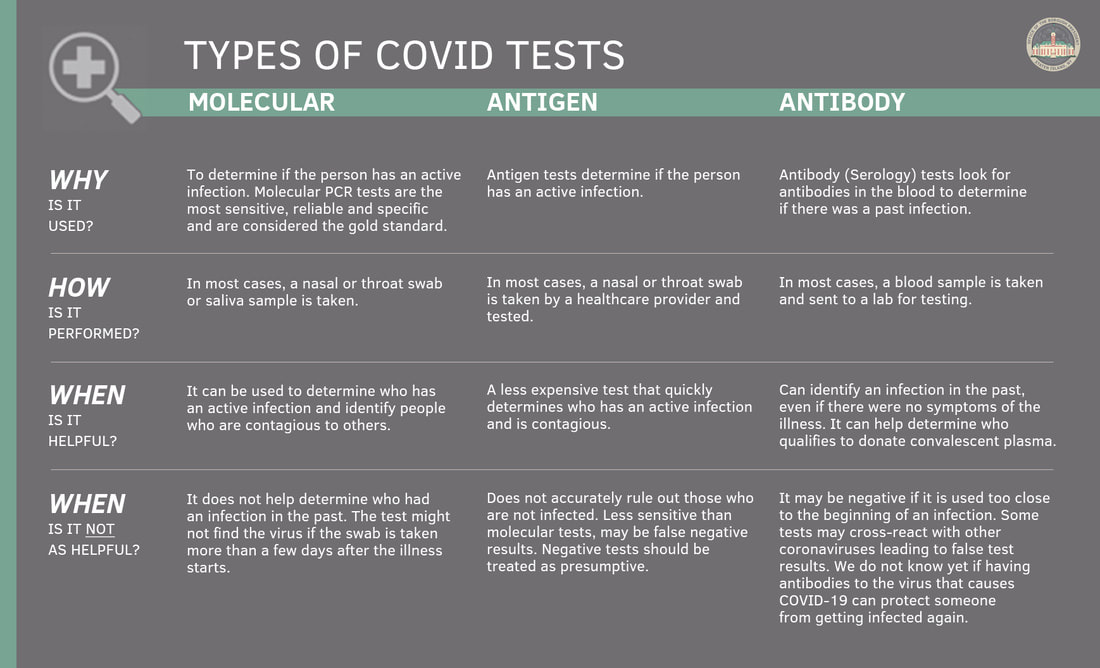
Testing or screening of symptom-free individuals is not covered. There are 2 types of COVID-19 tests.

Cincinnati Va Hosts Tent Mobile Unit To Prep For Covid 19 Spread
This requirement not only includes the cost of the test itself but also the cost of any related office urgent care emergency room or telehealth visits.
Does va insurance cover covid testing. Patients with insurance should not have any out-of-pocket costs for a covered COVID-19 test but you should check with your health plan to confirm before scheduling a test. The Virginia Department of Health VDH cares about you and your familys health. Review the summary list by date for COVID-19 test results performed.
The preference is to leave this to Government Test Centres and local NHS GPs. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently. Tricare like other insurance providers and the Department of Veterans Affairs VA only authorizes tests.
Testing is free with insurance plus a 35 charge for next-day results or 75 for same-day results. Those who previously paid a copay related to COVID-19 testing may file for reimbursement. Diagnostic tests determine if you are currently infected with COVID-19.
COVID-19 test results from any lab test ordered by a VA health care team will appear in your My HealtheVet account. Most people who have had close contact with someone known or suspected to have COVID-19. VDH strongly recommends COVID-19 testing for the following people.
Covid and antibody tests are not. CareFirst covers medically necessary COVID tests. Tricare will now waive co-pays for approved testing and office visits.
Well cover the basics of getting a COVID-19 test for travel and planning your trip accordingly. Treatment should still be obtained at a facility in our network unless it is an emergency. Select View More under VA ChemistryHematology.
116-136 requires most private health insurance plans to cover COVID-19 testing administration of the test and related items and services as defined by the acts. CareFirst does not pay for COVID-19 diagnostic testing for return to workschool testing. At this time were not charging a copay for testing.
Worksite Labs conducts tests in Ft. The COVID-19 test itself is free for veterans enrolled with VA or Tricare. CareFirst will fully cover the cost of emergency use authorized home COVID-19 testing when ordered by a doctor nurse practitioner or other authorized provider.
Insurers are legally required to pay for in-network testing so try to find a medical facility where you know youll be covered. For patients who test negative for COVID-19 through a rapid test and come into the clinic the clinic visit should be considered. Your diagnostic test and in-person visit to diagnose COVID-19 will be covered by your plan.
COVID-19 testing at VA We offer diagnostic testing for Veterans who are enrolled in VA health care and meet the CDC testing criteria. Many insurers have also agreed to cover the cost of a COVID test if its done at an out-of-network facility but youll want to reach out to your insurance company or MedicareMedicaid provider before your visit. Because serological tests for COVID-19 meet the definition of in vitro diagnostic tests for the detection of SARS-CoV-2 or the diagnosis of COVID-19 serological tests are covered by TRICARE if they are determined to be medically necessary To be medically necessary means it is appropriate reasonable and adequate for your condition.
Many popular destinations are opening the gates to visitors as long as they can show proof of vaccination or a recent COVID-19 test that proves theyre free of infection. We cover without member cost sharing a same day office emergency room or other provider visit at which a COVID-19 test is ordered or administered. Both the FFCRA and the CARES Act contain requirements that group and individual health insurance plans cover COVID-19 diagnostic testing without cost-sharing co-pays or deductibles.
This includes any doctors outside of our network. If you have health insurance you must bring your card with you to the test site. Has no plans to include COVID19 or Antibody testing.
Coronavirus disease 2019 COVID-19 antibody test. Military family members and retirees covered under Tricare and veterans using the Department of Veterans Affairs health system can receive a test for the novel coronavirus formally known as COVID. Medicare Part B Medical Insurance Part B covers certain doctors services outpatient care medical supplies and preventive services.
What COVID-19 Testing Will Tricare Cover. The guidance documents explain that the mandate to cover testing with no cost-sharing applies to all types of COVID-19 diagnostics PCR tests antigen detection tests and serology tests. In-network Urgent CareRetail locations if.
Select Labs Tests on the home page. Please note that this information is current as of August 2021. Eligible Veterans will not be charged a copayment for COVID-19 viral testing.
116 127 as amended by the Coronavirus Aid Relief and Economic Security Act CARES Act. We encourage you and your health care provider to use FDA-authorized tests. COVID -19 TestingThe Families First Coronavirus Response Act FFCRA.
Covers a COVID-19 antibody or serology test. VA will reimburse community providers for COVID-19 viral testing of eligible Veterans at one of the following outlets. People with symptoms or signs of COVID-19 regardless of vaccination status.
There will be no cost-sharing including copays coinsurance or deductibles. The cost is 90 for results in 24 hours or 150 for results in 12 hours. Testing for COVID-19 is important to slowing the spread of COVID-19.
Covid Testing LLC does testing at several locations in Orlando and Central Florida. Lauderdale West Palm Beach and Miami. Federal law requires insurers to fully cover coronavirus tests ordered by health care providers meaning the doctor cannot apply a deductible or co-payment to the service.
If as part of that visit the provider administers or orders a test for influenza strep or other respiratory infection that additional testing will also be covered without member cost sharing. Testing required as part of outpatient day patient or inpatient treatment is covered. Sign in to your account and follow these steps to access your COVID-19 test results.
When you travel and youre forced to quarantine because of Covid you should know whether your travel insurance policy covers you.

Covid 19 Get Tested City Of Alexandria Va

Gsa And The Va Update Covid 19 Vaccination Requirements Timelines And Testing Rules Insights Holland Knight

Urgent Care Covid 19 Testing Telehealth Patient First Fairfax
/cloudfront-us-east-1.images.arcpublishing.com/gray/GZYXYQYUUZDIJBOHB7O2GFD6HE.png)
Free Walgreens Drive Thru Testing Site To Open Aug 7
Mobile On Site Covid 19 Testing Near Me Express Healthcare Llc

Urgent Care Center Of Arlington Urgent Care Arlington Va

Covid 19 Get Tested City Of Alexandria Va
Medicaid Emergency Authority Tracker Approved State Actions To Address Covid 19 Kff
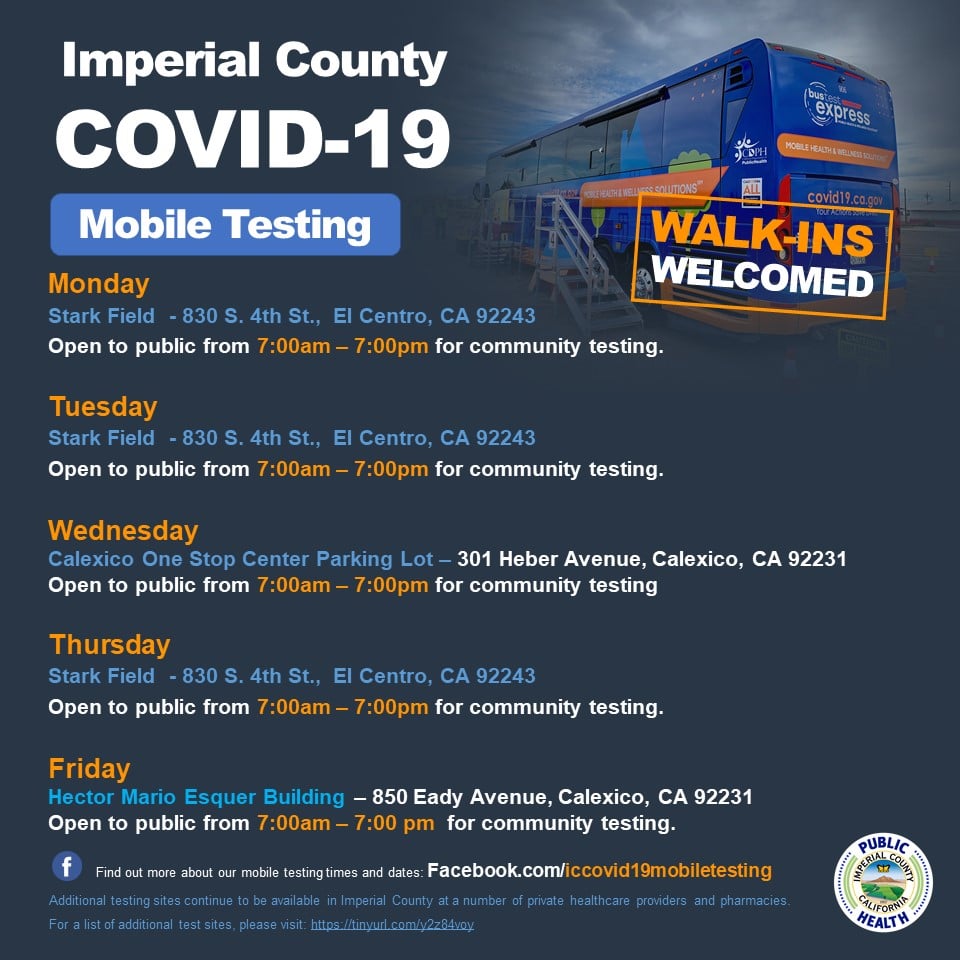
Covid 19 Testing Imperial County Public Health Department
Covid 19 Testing Imperial County Public Health Department
Two Positive Covid 19 Cases Reported At W Va Jails Officials Say First Report Was Inaccurate Health Register Herald Com
Vaccine Coverage Pricing And Reimbursement In The U S Kff

Where To Find Covid 19 Testing In Indianapolis

Covid 19 Testing Faqs In College Park New Carrollton Md And Falls Church Va
Vaccine Coverage Pricing And Reimbursement In The U S Kff

Va Health Care Cost And Co Payments Military Com


Posting Komentar untuk "Does Va Insurance Cover Covid Testing"