Does Empire Blue Cross Cover Rapid Covid Testing
Find a COVID-19 testing location near you by using this tool. Blue Shield will waive copays coinsurance and deductibles for COVID-19 treatments received between March 1 2020 February 28 2021.

More Sites To Conduct Covid 19 Rapid Tests Northwell Health
Cost for testing.

Does empire blue cross cover rapid covid testing. COVID-19 vaccines reduce the risk of severe disease hospitalization and death and slow spread of the virus. However we do cover the cost of testing if a health care provider orders an FDA-approved test and determines that the test is medically necessary. Category Information you need to know Temporary changes Refer to the.
16 2021 1. Earn 50 when you get vaccinated by September 6. Independence covers the cost for medically appropriate diagnostic and antibody testing that is ordered by a physician or authorized by a health care professional at no cost to the member.
If youre traveling youll want to visit. That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs. A doctor must order a COVID-19 test for you.
If youre uninsured the government pays for your test. Charges may apply for COVID-19 testing services for travel. For Medicare Plus BlueSM and BCN AdvantageSM members follow Centers for Medicare Medicaid Services guidance.
Now you can earn 50 on your MyBlue Wellness Card when you receive at least one dose by September 6. If a GP doctor referral is required for a private testing clinic ask whether you will be charged for the referral. All Anthem plans cover medically necessary COVID-19 testing and the care visit where the test takes place with no out-of-pocket costs.
Aetna does not require a physicians referral to cover Covid-19 testing. COVID-19 testing performed at approved locations and following Centers for Disease Control and Prevention CDC guidelines. Empire Blue Cross Blue Shield which covers 4 million New Yorkers does said spokeswoman Alessandra Simkin.
COVID-19 testing for travel clearance purposes is conducted at private pathology clinics only. This includes hospital admissions for COVID-19 that began during this timeframe. An insured person can get a COVID-19 test PDF.
Billing tips for COVID-19 at a glance Revised Sept. Blue Cross and Blue Shield Companies Announce Coverage of Coronavirus Testing for Members and Other Steps to Expand Access to Coronavirus Care CHICAGO -- Blue Cross Blue Shield Association BCBSA announced today that its network of 36 independent and locally-operated Blue Cross and Blue Shield BCBS companies will waive prior authorizations and increase coverage for COVID-19 as. Through May 31 all BCBS companies including the BCBS Federal Employee Program FEPare.
Waiving cost-sharing for COVID-19 testing and treatment. For any new treatments received after February 28 2021 standard out-of-pocket costs will apply based on your plans benefits. In accordance with current regulations UnitedHealthcare will waive Empire Plan member copays coinsurance and deductibles for.
This coverage is in accordance with federal mandates through the end of the public health emergency. Empire Blue Cross Blue Shield which covers 4 million New Yorkers does said spokeswoman Alessandra Simkin. The best way to prevent infection is to get a COVID-19 vaccine.
BCBSTX is waiving your share of the costs for COVID-19 testing and testing-related visits until the end of the Health and Human Services COVID-19 public health emergency order. Independence Blue Cross Independence covers the cost of administering vaccines with no cost-share such as co-pays deductibles coinsurance for members regardless of where the vaccine is given. The FDA has authorized three vaccines that have proven to be up to 95 effective in protecting against COVID-19.
For Blue Cross commercial and BCN commercial members follow the guidance in this document. Does Independence cover COVID-19 testing. Aetna does not require a physicians referral to cover Covid-19 testing.
No Blue Cross doesnt cover the cost of workplace or occupational screening tests for COVID-19. UnitedHealthcare will cover FDA-authorized rapid point of care virusantigen detection and antibody testing. Empire will cover the COVID-19 vaccine.
UnitedHealthcare is also waiving cost sharing for COVID-19 testing-related services received in-person or via telehealth for the following health plans. Check the CDC website for up-to-date information. Coverage for rapid test kits aligns with coverage for other COVID-19 diagnostic testing under federal law.
This applies to all members regardless of the type of health plan they have or which doctor or healthcare professional they choose to visit for COVID-19 vaccination. Help speed access to COVID-19 testing and treatment and encourage the use of telehealth instead of in person visits to stop the spread of COVID-19. Yes Blue Cross Blue Shield members will not have to pay for COVID-19 diagnostic tests that are performed by a licensed or authorized health care provider through October 18 2021 Exclusions to this coverage include testing for the following.
July 6 2021. Premera Blue Cross is here to support members employers and healthcare providers during the coronavirus COVID-19 outbreak. There are no out-of-pocket costs for COVID-19 testing at a testing site.
Please talk to a doctor first to be certain you need a COVID-19 test. COVID-19 testing is available at no cost. Getting tested for COVID-19 is free convenient and easy.
Due to overwhelming interest in our new COVID-19 Vaccination Incentive Program we are extending the deadline for your first dose of a COVID-19 vaccine. This is a pdf file when needed by any provider in or out of their health plan network at no cost. If rapid testing is provided by or with a referral from a licensed or authorized healthcare provider it is a covered benefit with no member cost sharing.
Rapid Point of Care Testing. Pharmacists may temporarily order and conduct COVID-19 diagnostic testing for Blue Cross Blue Shield members at New York State pharmacies through July 5 2021 Please contact Blue Cross Blue Shield at 716 887-2054 or 1-800-666-4627 for questions on submitting claims for COVID-19 testing to review qualifications and requirements. Lab tests to diagnose COVID-19 are covered at no cost.
Empire members wont have out-of-pocket costs for the vaccine during this national public health emergency. Updates as of September 30 2021 Prior authorization requirements waived for transfers to home health or SNF facilities through October 31 2021. Therefore Blue Cross plans will cover outpatient COVID-19 testing and treatment as well as all telehealth visits without charging members any.
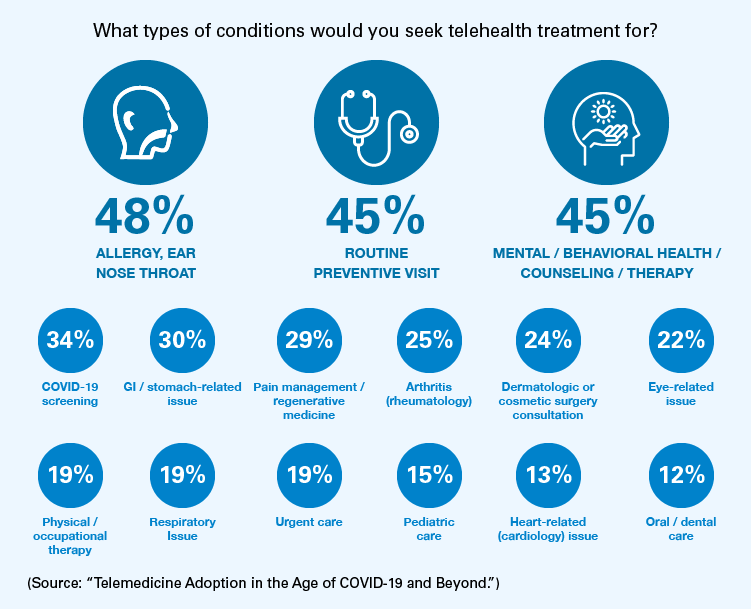
Increasing Telehealth And Virtual Care In The Covid 19 Era Blue Cross Blue Shield

Carefirst Bluecross Blueshield To Cover All Costs For Covid 19 Vaccines Healthcare Finance News
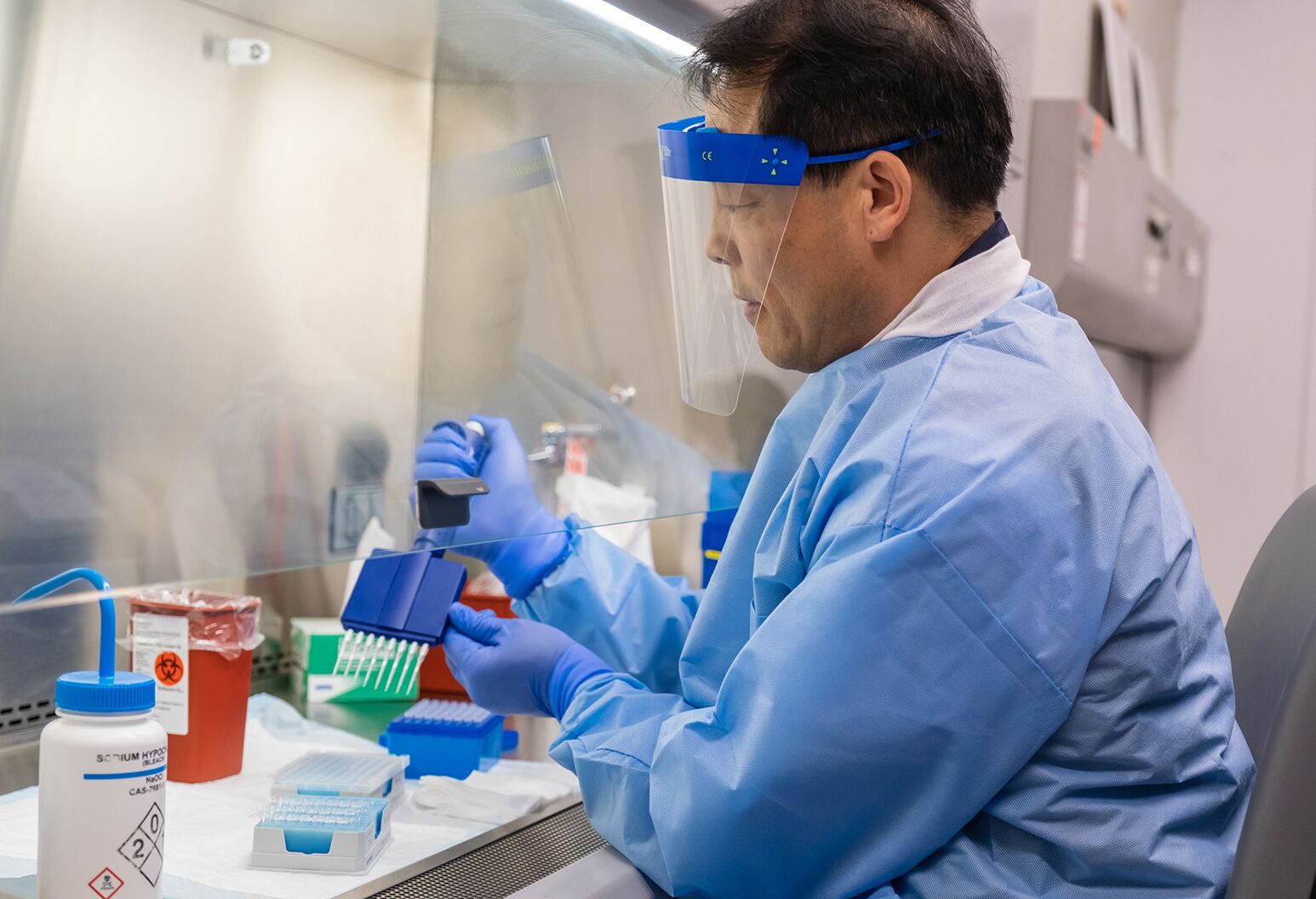
Northwell Expands Testing To Aid Covid 19 Recovery Northwell Health

Blue Cross Coverage Of Covid 19 Testing What To Know Mibluesperspectives
Coronavirus Covid 19 Information For Individual Family And Employer Group Plans Empire Bluecross Blueshield
Find A Coronavirus Covid 19 Testing Site Anthem
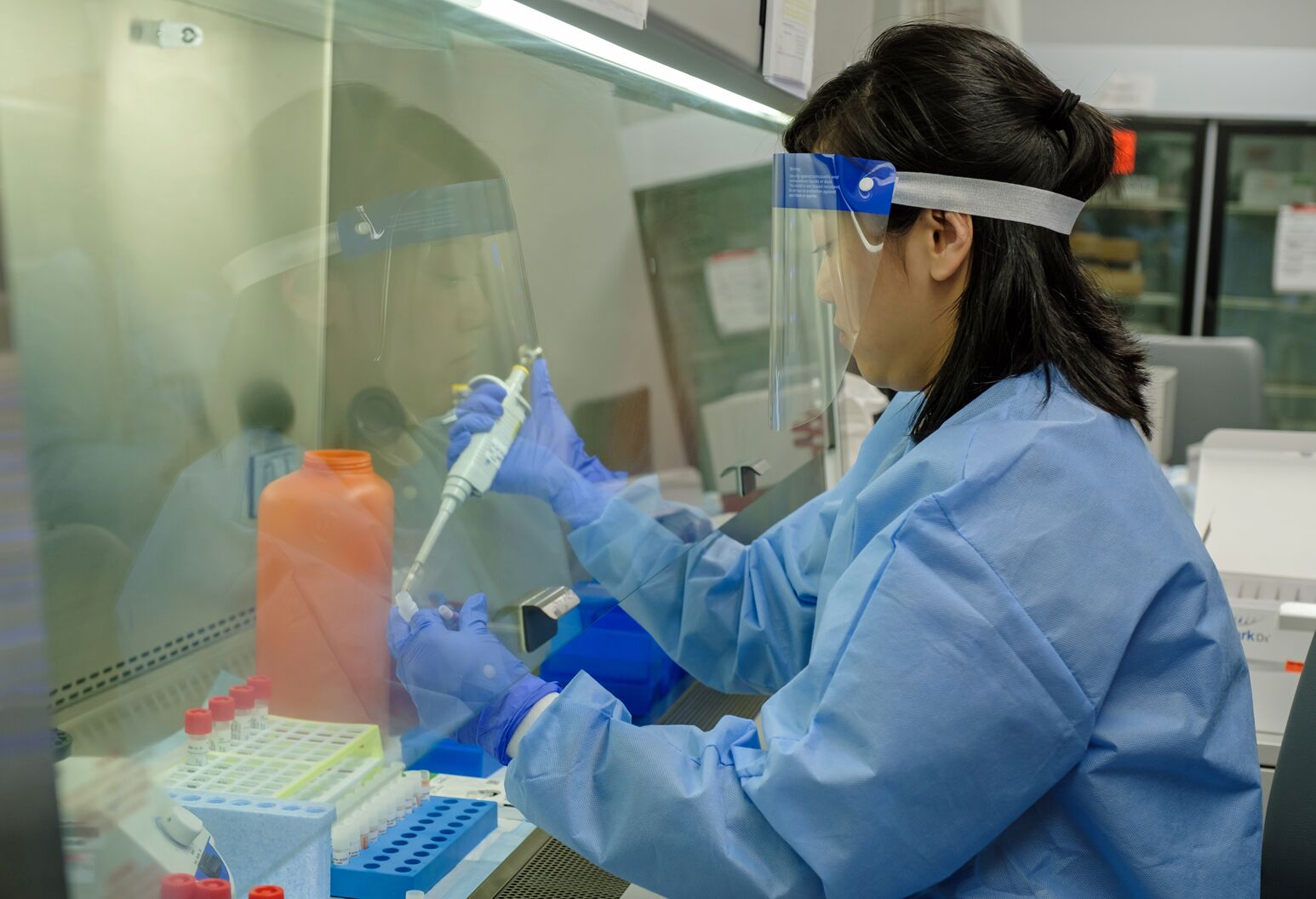
Northwell Labs Begins Semi Automated Testing For Covid 19 Northwell Health

Coronavirus Covid 19 Information For Individual Family And Employer Group Plans Empire Bluecross Blueshield

Coronavirus Covid 19 Resource Center Empire Bluecross Blueshield

Northwell Opens Covid 19 Testing Sites In Huntington Riverhead Northwell Health
Coronavirus Covid 19 Resource Center Empire Bluecross Blueshield

Covid 19 Testing Your Options And Telehealth S Role Amwell

Testing For Covid 19 Faqs Blue Shield Of Ca

Covid 19 Testing Bills Surprise New Yorkers Crain S New York Business
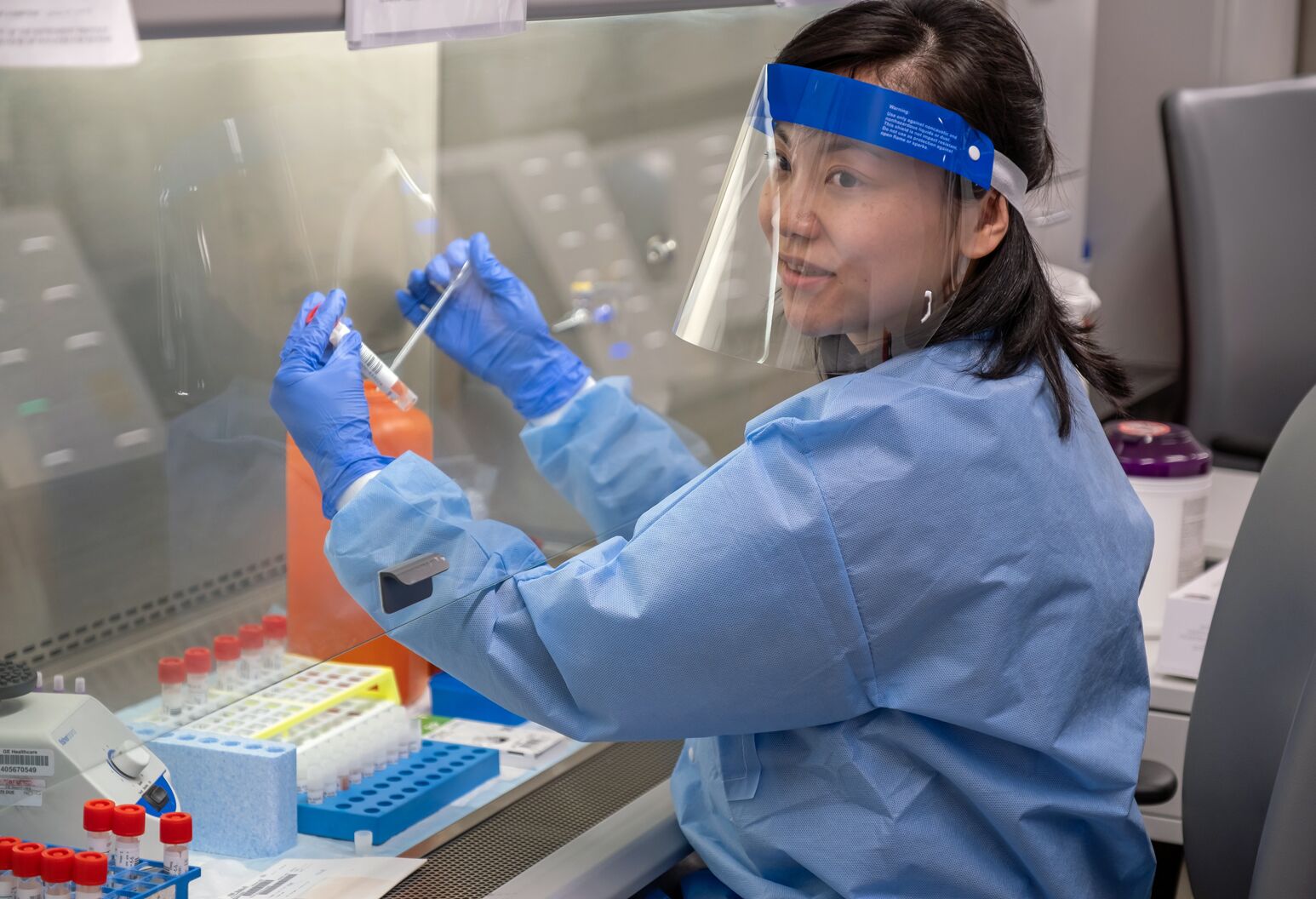
What S In A Covid 19 Test Northwell Health

Coronavirus Covid 19 Resource Center Empire Bluecross Blueshield

Empire Blue Cross Blue Shield Rehab Coverage Crest View Recovery


Posting Komentar untuk "Does Empire Blue Cross Cover Rapid Covid Testing"