Does State Insurance Cover Rapid Covid Testing
If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. The cost is 90 for results in 24 hours or 150 for results in 12 hours.

Covid 19 Rapid Testing In Ny Bioreference Laboratories
Shots - Health News Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show.

Does state insurance cover rapid covid testing. Medicare covers these tests at different locations including some parking lot test sites. Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test. The Department of Health and Human Services offers a COVID-19 test center locator.
You will need an appointment for most of these sites. Can I go to a temporary or pop-up COVID-19 testing site. State variations and regulations may apply.
Your plan will cover diagnosis testing and treatment associated with COVID-19 including. Many airports are now offering test sites. Federal law requires insurers to fully cover coronavirus tests ordered by health care providers meaning the doctor cannot apply a deductible or co-payment to the service.
Check back often for updates. Covid Clinic provides 0 upfront service for COVID-19 PCR testing. BCBSIL is waiving your share of the costs for COVID-19 testing and testing-related visits until the end of the Health and Human Services COVID-19 public health emergency order.
UnitedHealthcare is updating testing guidelines coding and reimbursement information for the COVID-19 health emergency based on guidance from the Centers for Medicare Medicaid Services CMS the Centers for Disease Control and Prevention CDC state and federal governments and other health agencies. Worksite Labs conducts tests in Ft. Waiving all prior authorization requirements for COVID-19 testing and related covered services.
When paying out-of-pocket for rapid testing patients may be able to receive reimbursement from their health insurance provider for all or a portion of their COVID-19 test. The Families First Coronavirus Response Act ensures that COVID-19 testing is free to anyone in the US including the uninsured. 2 Rapid-result tests can be pricey costing up to 250 and often arent covered by health insurance.
We cover without member cost sharing a same day office emergency room or other provider visit at which a COVID-19 test is ordered or administered. The rapid test at Walgreens is listed at 49 total. Commonly known as COVID-19 PCR test or simply PCR the State Health Plan covers this test at no member cost when prescribed by a healthcare provider for individuals who are symptomatic and for those who have been exposed to COVID-19 and are concerned about infection for the purpose of identifying and treating the.
Lab tests to diagnose COVID-19 are covered at no cost. You might consider buying travel insurance coverage for personal or leisure travel. Lauderdale West Palm Beach and Miami.
Some that charge travelers for rapid and PCR tests and some that offer complimentary screenings for travelers. Covid Testing LLC does testing at several locations in Orlando and Central Florida. If you go to an out-of-network doctor or provider to get tested for the coronavirus COVID-19.
If you have health care coverage directly from an insurance company the health insurance marketplace or through your employer including through COBRA. Insurers not required to pay for mandatory employer COVID-19 tests HHS says New guidance also covers telehealth coverage and balance-billing for testing-related services. No-cost testing is in accordance with Federal and State waivers guidelines.
The cost of a COVID-19 test should be fully covered by health insurance. Local or state public health authorities. State Says New Guidance Clarifies That COVID-19 Test Costs Should Be Covered by Health Insurance.
A test must be covered if your attending health care provider has assessed your individual situation and determined that it is medically appropriate you have symptoms or have a known or likely recent exposure to COVID-19. That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs. 2 Walgreens website listed its additional charge as 29 and CVS listed a 39 extra charge for the PCR test.
You may also have to fill out a screening. When tests are available for you in your state Medicare covers and you pay nothing for. Waiving cost-sharing for COVID-19 testing and treatment.
If as part of that visit the provider administers or orders a test for influenza strep or other respiratory infection that additional testing will also be covered without member cost sharing. Contact your health care provider or your state or local public health department for more information. Testing is free with insurance plus a 35 charge for next-day results or 75 for same-day results.
Learn more about how the additional ways Medicare is helping cover beneficiaries during the coronavirus pandemic. We cover without member cost sharing a same day office emergency room or other provider visit at which a COVID-19 test is ordered or administered. C ontact your insurance company.
Tests to diagnose or aid the diagnosis of COVID-19. Additional testing sites may be available in your area. To find a testing facility near you just select your state from the dropdown menu or scroll down to your respective state to see your options.
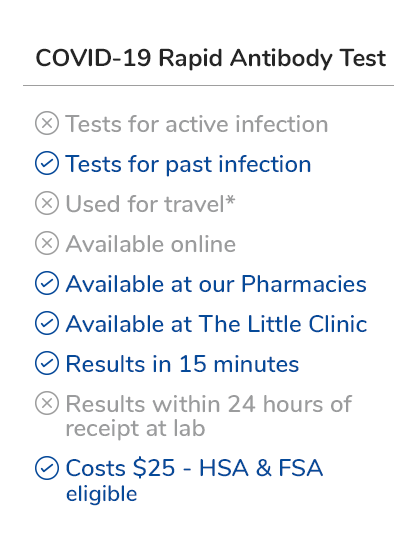
Currently testing for COVID-19 is covered by the Plan as follows. As of Wednesday Dec. Your diagnostic test and in-person visit to diagnose COVID-19 will be covered by your plan.
If as part of that visit the provider administers or orders a test for influenza strep or other respiratory infection that additional testing will also be covered without member cost sharing. COVID-19 testing at temporary or pop-up testing sites is covered by Blue Shield and Blue Shield Promise without out-of-pocket costs. It Depends.
COVID Testing Coverage TRICARE covers COVID-19 tests ordered by a TRICARE-authorized provider An authorized provider is any individual. This includes any doctors outside of our network.

Covid 19 Testing And Faqs First Call Urgent Care

Negative Covid 19 Test Required For Travel To The United States Beginning January 26 U S Embassy Consulates In Russia

Where Can I Get A Covid Test In Cancun The Riviera Maya
What Is A Rapid Antigen Test How Is It Different From Other Covid 19 Tests Abc News

How Home Coronavirus Testing Could Slow Disease Spread

Covid 19 Igm Igg Antibody Rapid Test Results In 10 Minutes
Rapid Covid 19 Tests Should Be Rolled Out In High Risk Settings But Not In The General Community Experts Say Abc News

Covid 19 Testing Information Travel Return To Work Complete Health Partners

New Covid 19 Rapid Drive Thru Testing Site Opening In South Tulsa
Pharmacy Hours Online Services Coronavirus Updates City Market
Nyc Test Trace Corps Launches Rapid Covid 19 Testing At Jfk Airport S Terminal 5 Nyc Health Hospitals

Covid 19 Testing And Covid Antibody Testing Stat Med Urgent Care

Austin Travis County Covid 19 Testing Where To Get Tested
Texas Medclinic Offers Rapid Covid Testing Near Me Walk In Clinic
What S In A Covid 19 Test Northwell Health
![]()
Covid 19 Test Prices And Payment Policy Peterson Kff Health System Tracker

Covid 19 Testing Sites City Of Lakeland
Pharmacy Hours Online Services Coronavirus Updates City Market

Posting Komentar untuk "Does State Insurance Cover Rapid Covid Testing"